Colorectal Cancer
Colorectal Cancer
Where does colorectal cancer come from?
Colorectal cancers start in the cells of the inner lining of the colon and rectum. Though there are many theories as to why these cells become cancerous, the two most common causes are thought to be due to genetics and the environment.
Cancers are thought to start as polyps that grow over 5-10 years before they become cancerous. That is why it is important to get a colonoscopy when indicated, even if you have no symptoms.
What is Colorectal Cancer?
Colorectal cancer refers to cancer in the lower digestive tract, also known as the large bowel or large intestine.
It is the 4th most common cancer in the US and the 2nd leading cause of cancer deaths.
There has been a steady decline for many years in the annual rate of deaths from colon cancer.
Though it is more common in older adults, there has recently been an increase in the rate of colon cancers seen in people under the age of 50.
What are the symptoms of colorectal cancer?
Blood in the stool
Changes in bowel habits for more than 2 weeks
Thinning of stools
Cramping
Pain and /or weight loss (less frequent)
Though the most common cause of rectal bleeding is from hemorrhoids, if you see bleeding, you should notify your primary care physician.
How is colorectal cancer diagnosed?
The most common way to diagnose colorectal cancer is with a colonoscopy. This is when a camera is passed through the anus and along the length of the colon. Since cancers start on the inside of the colon, it can detect not only cancers but even polyps that may eventually grow into cancers.
If cancerous tissue is identified:
A biopsy is taken from the growth and sent for testing to confirm that it is cancerous.
Results take 3 to 10 days.
A colonoscopy is the best way to screen for and diagnose colon cancer.
What happens once I am diagnosed with colorectal cancer?
The biopsy can confirm that the growth is cancerous, but it can not tell anything about the stage of the cancer.
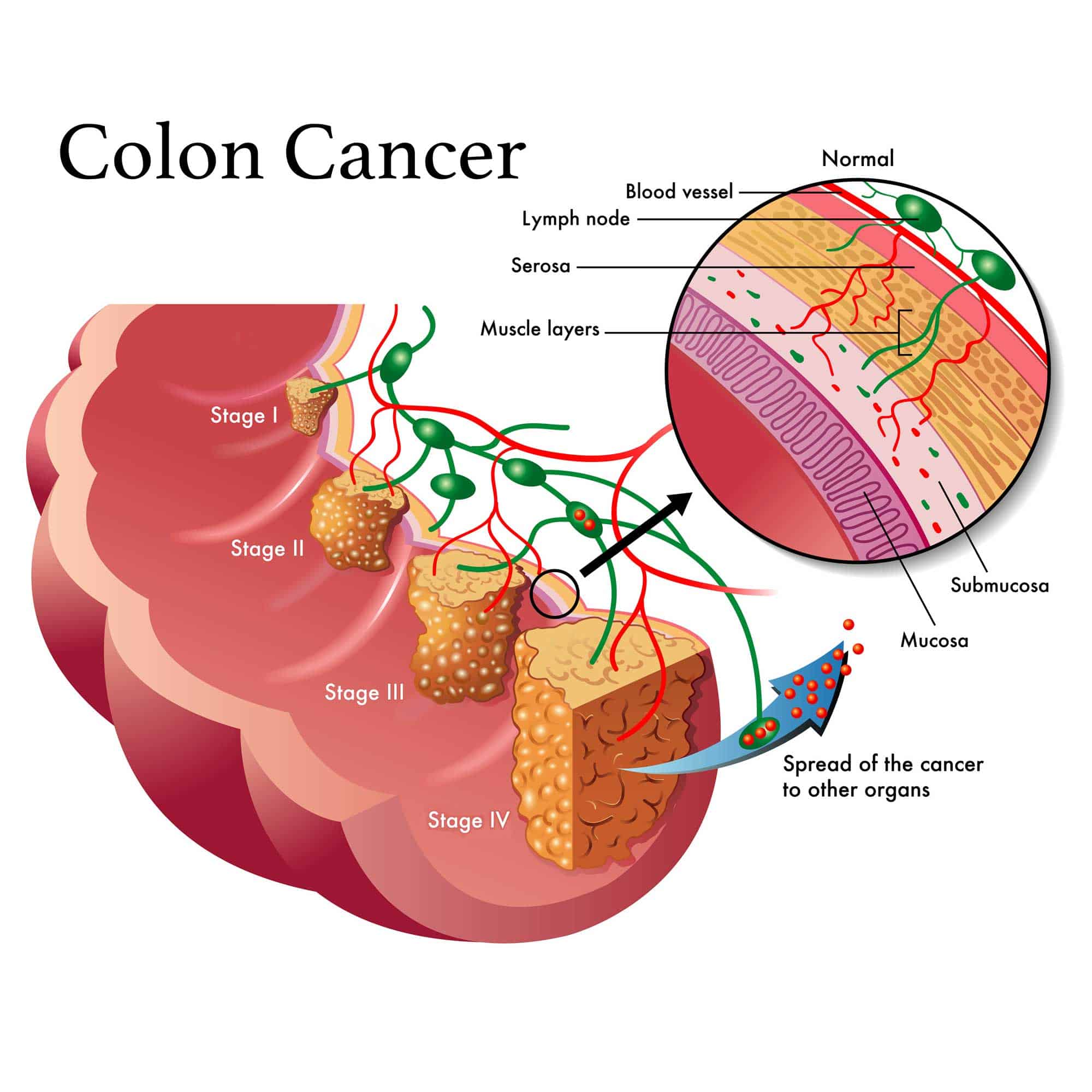
Staging refers to how much the cancer has spread. The exact stage often can’t be known until surgery, but imaging studies can usually give a good idea of the stage.
Once the diagnosis is made, a CT scan of the chest, abdomen, and pelvis is typically performed as the next step to look for any spread within the body.
MRIs are often ordered for rectal cancers in addition to a CT scan. This looks for any spread outside the wall of the rectum.
PET scans show little benefit in understanding the initial staging of colorectal cancers, but there are instances when this is helpful and is sometimes ordered before or after surgery.
Once this information is obtained, a decision is made to proceed either with surgery first or with chemotherapy and/or radiation.
Does surgery mean a colostomy bag?
The majority of the time, surgery can be performed without the need for a colostomy bag. When a colostomy bag is necessary, sometimes it is temporary, but this decision is made on an individual basis. Colorectal surgeons go through specialized training and are skilled at removing cancers and avoiding permanent colostomies as much as possible. The primary goal of any cancer surgery is to first remove all the cancer, and the next priority is to avoid a colostomy if at all possible.
Will I need chemotherapy or radiation?
For colon cancers, chemotherapy is given based on the stage of the cancer.
If the tumor is contained within the bowel (stage 1 or 2) chemotherapy is generally not recommended.
If cancer cells are found in the lymph nodes on examination by the pathologist (stage 3) then chemotherapy is generally recommended. This does not mean that any cancer has been left behind, but it helps decrease the chance of the cancer coming back.
If the tumor has spread to other organs such as the liver, this is considered stage 4. In those cases, chemotherapy is usually given before surgery if possible. Radiation is seldom recommended for colon cancers of any stage.
For rectal cancers, chemotherapy and radiation may be recommended for certain cancers that appear to be growing or spreading outside the rectal wall. That is why an MRI, as well as a CT scan, is done first before any treatment. Chemotherapy and radiation are done before surgery to shrink the tumor and minimize the chance of recurrence after surgery is performed. This is a major difference in treatment between colon cancers and rectal cancers. Rectal cancers that are contained completely within the recall wall, will usually go to surgery first. Recent evidence has found that certain rectal cancers that appear to go away completely with just chemotherapy and radiation, can avoid surgery altogether but there needs to be very close observation done on these select patients.
What does surgery involve?
The vast majority of surgeries can be performed with minimally invasive techniques, which means laparoscopically or robotically.
Usually, a bowel prep is given the night before, similar to a colonoscopy. The surgery is done under general anesthesia and usually takes a few hours.
During surgery, a section of the large intestines with the tumor will be removed and the two ends of the bowel will be reattached.
Lymph nodes that are along the colon and near the tumor are also removed. This is sent to a Pathologist who looks at all of the tissue removed over the next several days and then reports on the stage of the tumor.
Recovery generally requires 1-2 days in the hospital.
The patient can go home once they are eating and feeling comfortable. Though most patients are moving their bowels by the time they go home, it is not always required.

